Patellofemoral Instability: not just a dislocating kneecap
Patellofemoral instability is a debilitating condition that frequently occurs in young, active people, significantly affecting their quality of life.
It can occur due to injury e.g. a direct impact to the knee, or from variations in a patient’s anatomy that allow the patella (kneecap) to dislocate with minimal force.
Patellofemoral instability, however, is not just a dislocating patella.
A person could experience knee pain, a locked knee, a patella that only partially dislocates (called a subluxing patella), or a patella that completely dislocates.
—– Read more about Patellofemoral Instability here —–
When a full dislocation occurs, the diagnosis is not difficult, but what about the other scenarios?
Dr Laurie Hiemstra, shares the following case examples of patients she has diagnosed and treated:
Case Example 1

An 18-year-old AAA hockey player with no history of knee injury is hit during a game.
He feels his kneecap dislocate. It is reduced (i.e. pushed back in place) by his trainer at the game. Xray’s demonstrate no bony abnormality. He rehabilitates his knee but still has difficulty playing because of feelings of instability.
This is a clear example of a traumatic onset of patellofemoral instability.
To treat his instability, his medial patellofemoral ligament (MPFL), the ligament that prevents the patella from dislocating, was reconstructed (a surgical procedure called an MPFL Reconstruction).
He was then able to rehabilitate and return to sport at 4 months with no further feelings of instability.
Case Example 2
A 16-year-old female soccer player presents with a ‘locked knee’.
The prior week, she played a two-day soccer tournament. While she did have a twisting type injury during one of the games, she was able to walk it off and keep playing, finishing the tournament. She only experienced some minor swelling afterwards.

She went to bed that night, and when she woke up in the morning, she was unable to straighten her knee.
Attempts to straighten the knee was associated with significant pain.
Physiotherapy was tried but did not help her symptoms. X-rays were taken and appeared normal. An MRI looked essentially normal with some slight increased signal in the ACL.
Arthroscopy (knee scope) showed a normal knee with some minor scuffing on one region of the patellar (the medial patellar facet). After the scope, she regained full range of motion of the knee but continued to have pain and a partially dislocating patellar.
To treat these symptoms, an MPFL imbrication was performed, where stitches were used to tighten the ligament.
She went on to have a complete recovery.
This case represents a difficult diagnosis of a single subluxation episode leading to a locked knee or ongoing knee pain.
Often, these patients are “sent to me as a meniscus tear or ACL tear despite normal MRI findings”. These patients, usually young girls, have had a patellar subluxation episode and their knee is functionally, not mechanically, locked.
The spectrum of Patellofemoral Instability
The presentation such as in Case Example 2, of an athlete during a sporting event is common but in the extreme case.
A sedentary person may also have knee pain with no remembered injury.
These patients often have multiple ligamentous laxity (MLL) or “loose” ligaments.
They may also have valgus alignment (knocked knees), or a shallow trochlea, where the groove that holds the kneecap is too shallow, allowing the patella to move too far side-to-side.
These patients may also have poor core stability or poor neuromuscular control of their knee extensors and adductors.
We have developed a mnemonic to help remember the spectrum of patients that present with patellofemoral instability.
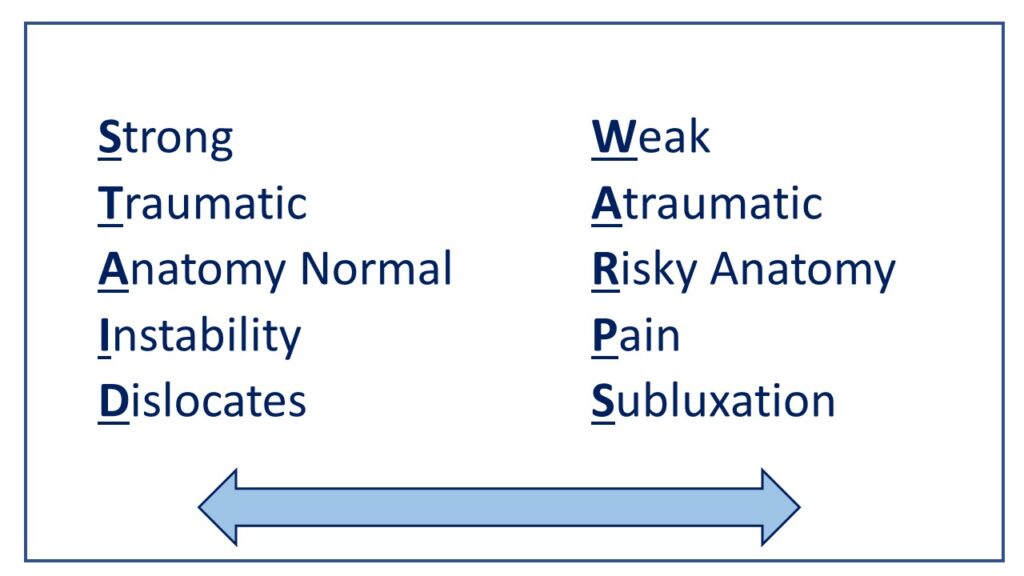
STAID: The patient with traumatic instability of the patella generally has strong hip and knee muscles and well developed quadriceps muscles. They have a traumatic origin to their instability. The anatomy is normal without predisposing factors. They complain of patellar instability and are clear that the patella dislocates or subluxes. If non-operative management fails, these patients do well with a MPFL reconstruction.
WARPS: The patients with atraumatic onset of symptoms generally have a weak core, knee extensors and hip muscles. They deny a traumatic event leading to their symptoms. They have anatomic factors that put them at risk of patellofemoral instability such as valgus alignment, trochlear dysplasia, rotational malalignment. They usually present with knee pain instead of instability and their inciting pathology is patellar subluxation.
Diagnosis and Treatment of the different types of Patellofemoral Instability
Diagnosis of patellofemoral instability in the WARPS group requires a high degree of clinical suspicion. The history of mechanism of injury tends to be very similar to an ACL tear but the symptoms will be quite different.
Both these patient groups will present with increased lateral laxity of the patella (it may be subtle) so they need to be examined from the end of the bed, supine, with leg relaxed and the lateral laxity of both patellae compared. They will all have apprehension during this maneuver.

In the STAID group, patients tend to have good muscle strength and standard rehabilitation will improve their symptoms.
In the WARPS group, I will trial some McConnell taping and a Patellar Stabilizer Brace. This usually improves their symptoms and will be both a diagnostic and therapeutic tool. Rehabilitation should be aimed at core, hip and knee extension muscle activation.
Often, because the WARPS patients are misdiagnosed as an ACL or meniscus, the rehab is too advanced and the patient is unable to complete the exercises due to pain. Simple quadriceps and hip exercises, in combination with electrical muscle stimulation (EMS) will improve their neuromuscular activation and allow them to advance to more complex exercises.
Contributing expert

Dr Laurie A Hiemstra, Orthopaedic Surgeon